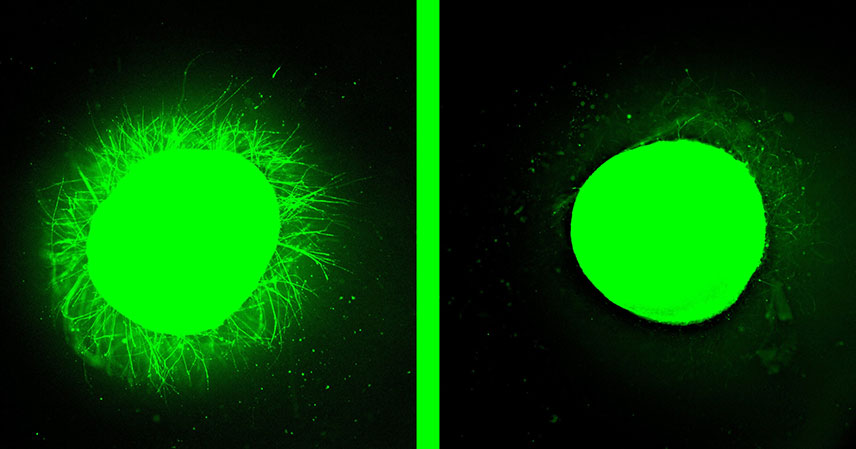
A groundbreaking development from Northwestern University scientists is poised to significantly accelerate research into spinal cord injuries. In a recent study, researchers unveiled the most advanced organoid model for human spinal cord injury developed to date. This innovative approach utilizes lab-grown human spinal cord organoids. These are miniature organs derived from stem cells. They meticulously simulate various injury types.
The study’s findings were published in the esteemed journal Nature Biomedical Engineering. They highlight the potential of these sophisticated models. They offer an unprecedented platform for understanding spinal cord damage. They also enable rigorous testing of promising new regenerative therapies. This advancement marks a crucial step forward in the quest for effective treatments.
Unpacking the Power of Spinal Cord Organoids 🌱
At the heart of this breakthrough are spinal cord organoids. These are not merely cell cultures. They are intricate, three-dimensional tissue structures grown in a lab from human stem cells. Essentially, they mimic the architecture and function of a real human spinal cord, albeit on a miniature scale. This fidelity to human biology makes them invaluable for research.
Traditional research methods have inherent limitations. Animal models, while useful, often fail to perfectly replicate human disease mechanisms. This is due to species differences. Two-dimensional cultures lack complex cellular interactions. They also miss the tissue organization crucial for understanding intricate conditions like spinal cord injury. Organoids bridge this gap. They offer a more accurate and human-relevant system.
The Northwestern team’s creation represents a significant leap in this field. They developed the “most advanced” model. They achieved a level of complexity and functional maturity. This allows for more realistic simulation of injury and repair processes. This enhanced realism is critical for translating laboratory findings into clinical applications more effectively.
Modeling Injury and Pioneering Therapy Testing 🔬
The true utility of these advanced organoids lies in their application. Researchers utilized the lab-grown models to simulate different categories of spinal cord injuries. This capability is paramount. Spinal cord injuries are not monolithic. They vary widely in their nature, severity, and affected neural pathways. Replicating these diverse injury profiles in a controlled environment is a powerful tool.
Crucially, the organoids served as a testing ground for a “promising new regenerative therapy.” Specific details of the therapy were not provided. However, the implication is clear. This platform allows for rapid and ethical evaluation of novel treatments. Such therapies could range from cell transplantation to innovative drug compounds. They aim to promote neural repair.
The ability to test therapies in vitro on human-derived tissue streamlines the drug development process. It allows scientists to quickly identify effective compounds. They can refine dosages and understand potential side effects at a foundational level. This efficiency could significantly shorten the timeline from discovery to clinical trials. This offers hope to many.
Implications for Future Treatments and Patient Care 🚀
This research carries profound implications for the future of spinal cord injury treatment. It is important to remember this is a preclinical development. However, it lays a robust foundation for future therapeutic breakthroughs. The enhanced understanding from these models could lead to more targeted interventions. These could benefit patients worldwide.
One major benefit is the acceleration of drug discovery. By providing a reliable human model, the organoids can help screen potential compounds. They do this much faster and with greater accuracy. This could lead to new treatments. These treatments would be specifically designed to repair damaged neural tissue. They aim to restore function and improve quality of life for individuals with spinal cord injuries.
Moreover, advanced human-derived models could reduce the reliance on animal testing. This aligns with ethical considerations. It also potentially yields more human-relevant results. The journey from lab bench to patient bedside is long and complex. But innovative tools like these organoids make that journey more efficient and hopeful.
Key Insights into Spinal Cord Research 💡
- Northwestern University has developed the most advanced human spinal cord organoid model to date. It offers unprecedented realism for research.
- These miniature, lab-grown organs are derived from stem cells. They allow scientists to accurately model various types of spinal cord injuries.
- The organoids provide a critical platform for testing novel regenerative therapies. This could accelerate the development of new treatments.
- This breakthrough promises to enhance our understanding of spinal cord injury mechanisms. It will also streamline the drug discovery process for future interventions.
In conclusion, the work by Northwestern University scientists represents a significant milestone. It impacts the field of regenerative medicine and neuroscience. By providing a sophisticated and human-relevant model, they have opened new avenues. These avenues explore the complexities of spinal cord injury. They also evaluate potential cures. This research instills renewed optimism for individuals affected by these devastating injuries. It highlights the power of scientific innovation to transform lives.
The path to clinical application is still ongoing. Yet, the foundation laid by this study is undeniably strong. It underscores the critical role of advanced organoid technology. This technology pushes the boundaries of what’s possible in health research. The scientific community eagerly anticipates further developments. These will undoubtedly stem from this pioneering work.
Source: Dancing molecules’ paralysis treatment heals lab-grown human spinal cord organoids